Baby eczema treatments on the NHS: A parent’s guide



Looking after a scratchy baby can be stressful enough, without feeling like you are fighting the healthcare system on your eczema baby’s behalf. While we have had a really good experience of baby eczema treatment with the NHS, much of this was down to the fact that our doctor’s little one also had baby eczema or atopic dermatitis, so he really understood the condition. But we know that not everyone is so fortunate in finding a GP who understands both the condition and the impact that it can have on the whole family. Understanding how the NHS intends to provide baby eczema treatments can really help in getting the right treatment for your baby’s eczema.
NHS baby eczema treatments are set out in the NICE guideline on Atopic Eczema in Children. This sets out the criteria for diagnosing baby eczema, the appropriate treatments and management techniques and when a child should be referred to an eczema specialist.
Our top tips for navigating baby eczema treatment on the NHS
- If you suspect your baby has eczema it is worth going directly to your GP, rather than starting with the health visitors. This is because the moisturisers which form the basis of all baby eczema treatments are available on prescription.
- In our experience, there is around a 50% chance that any given cream will work for any one baby. Even if a cream works well initially the benefits may reduce over time. So it’s useful to realise that the NHS is largely reactive. Your doctor will assume that prescribed treatments are working well unless you tell him or her otherwise.
- It’s worth knowing that not all doctors are particularly sympathetic when confronted by a case of baby eczema. This is largely because it typically clears up of its own accord before a baby’s first birthday.
- The skin is a complicated organ which isn’t always covered thoroughly in a GP’s training or training updates. If you are registered at a large practice it is worth asking if any of the doctors have a particular interest in skin conditions.
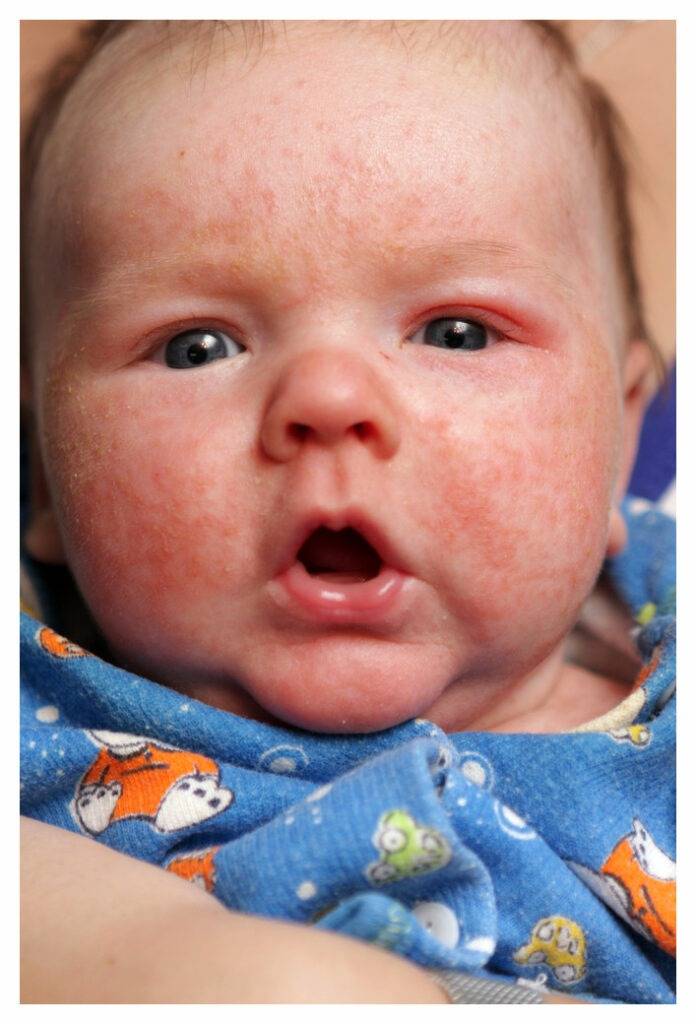
Diagnosing Baby Eczema
The key indicator in the diagnosis of baby eczema or atopic dermatitis is itchy skin. As babies can’t tell you that they are itchy, this is usually indicated by babies scratching themselves repeatedly. For an eczema diagnosis to be given, this itching needs to be coupled with at least 3 of the following:
- an obvious rash on the cheeks, trunk or extensor areas (the parts of the skin that touch when a joint bends are called the flexor surfaces, and the parts of the skin on the opposite side of the joint are called the extensor areas). In children over 18 months these rashes typically shift to flexure areas, usually behind the knees and inside elbows;
- a history of rashes on cheeks or extensor areas (or flexure areas in toddlers and older children);
- history of dry skin; and
- a history of hayfever, eczema or asthma (known collectively as atopic diseases) in an immediate relative. For children over 4, this changes to a personal history of atopic diseases.
Matching treatments to eczema severity
The NHS aims to match the treatment to the severity of a baby’s eczema. We’ve tried to capture the spectrum of diagnosis and treatment in our ‘Baby Eczema NHS Treatment Summary’ below. Atopic Dermatitis, or Eczema, is a very changeable condition so it is common for a child’s eczema to move up (or down) the severity spectrum. Therefore condition should be monitored and their treatments changed accordingly.
The ScratchSleeves Summary of NHS Eczema Treatments
| Increasing Severity>>> | Clear | Mild | Moderate | Severe |
|---|---|---|---|---|
| Physical symptoms | Normal skin, no evidence of active eczema | Areas of dry skin, infrequent itching (with or without small red/discoloured patches) | Areas of dry skin with frequent itching and redness/discolouration (with or without evidence of scratching or skin thickening) | Widespread areas of dry skin, incessant itching, redness/discolouration with or without scratching, extensive skin thickening, bleeding, oozing, cracking, alteration of skin pigmentation |
| Psychosocial symptoms | No impact on daily life | Little impact on daily life, sleep or wellbeing | Moderate impact on daily activities and psychosocial wellbeing, frequently disturbed sleep | Severe limitation of daily activities and pyschosocial functioning. Nightly loss of sleep. |
| GP treatments | Emollients for maintenance | Emollients and mild topical steroid creams (e.g. 1% hydrocortisone) | Emollients and moderate topical steroid creams | Emollients and stronger topical steroid creams |
| Specialist treatments | Stronger topical steroid creams, bandages (e.g. wet or dry wraps), calcineurin inhibitor creams | Calcineurin inhibitor creams Bandages (e.g. wet or dry wraps) Phototherapy Systemic and biologic drugs |
More on Baby Eczema treatments
Emollients
These medical moisturisers and form the basis of all eczema treatments. They aim to reduce the moisture lost by the skin by covering it in a protective layer as well as replenish the skin’s moisture content. They are available as creams and bath additives and there is a plethora of different brands available on prescription. It is a case of trial and error to find one that works for your baby’s eczema. However, some children can develop a sensitivity to particular emollients over time. If your baby’s eczema seems to be getting worse it’s worth asking your GP for a different emollient. These sensitivities can settle after a break so you may end up alternating between 2 or 3 different brands. Emollients need to be used regularly and liberally, and cannot be over-used. Read more here.
Corticosteroid creams
Corticosteroid creams, also known as ‘steroid creams’ or hydrocortisone, are used to reduce skin inflammation and irritation. While they do not cure eczema, they can provide much needed relief during flare-ups. They also give you and your doctor some time to identify the triggers for your baby’s eczema. They should only be used for limited periods but are safe and should have no adverse effects if used as you GP instructs. Read more here.
Antihistamine
Antihistamines (e.g. Children’s Priton) can prescribed to reduce itching and help itchy babies sleep during eczema flare-ups. However they are not used in the day-to-day management of baby eczema.
Calcineurin inhibitor creams
These act on the immune system to reduce skin inflammation by blocking a chemical (calcineurin) which causes redness and itching of the skin. Like corticosteroid creams, they won’t cure eczema but they reduce the itching and inflammation, however these creams are only licensed for children over the age of 2.
Food allergies
The NICE guidelines indicate that a food allergy should be considered in babies and young children with moderate or severe atopic eczema that has not been controlled by optimum management, particularly if the child has (or has had) colic, persistent vomiting or failed to thrive. A trial period on a dairy-free formula milk can be prescribed.
Bandages, phototherapy and systematic therapies
Bandages, phototherapy and systematic therapies are generally prescribed by specialist dermatology units and should only be used under medical supervision and monitoring. Improperly used, these therapies can aggravate rather than alleviate baby eczema.
Referral to NHS eczema specialists
Most cases of baby eczema/atopic dermatitis are successfully treated by parents and GPs using emollients, corticosteroids and, most importantly, by identifying and avoiding eczema triggers. However, some cases are more severe or slow to respond and need specialist treatment. The NHS eczema specialists work as hospital based multi-disciplinary teams usually made up of:
Eczema nurses. Referrals to specialist eczema nurses are usually for demonstrations on how to use emollients and bandages effectively. Eczema nurses will also carry out regular treatment reviews for little ones who have previously been seen by a dermatologist. The eczema nurses are the backbone of NHS eczema services. They are senior specialist nurses, specially trained to deal with skin conditions and allergy testing. It’s worth remembering that they are part of a multi-disciplinary team and will know when something needs to be referred on to a specialist doctor (and be able to make that referral). A lot of the more experienced ‘eczema parents’ we talk to actually prefer appointments with the eczema nurses over those with dermatologists.
Dermatologists. You can expect a referral to a dermatologist for severe baby eczema that is not responding well to emollient and corticosteroid treatments. This would include a child who is having 1-2 flares a month or who is reacting to badly to a number of emollients. Referrals can also be made for babies with severe or recurrent eczema infections. They can also be made if eczema is causing significant social or psychological problems for a child or their carers. This includes regular sleep disturbance, or for older children poor school attendance.
Allergy specialists. If an allergy is suspected to be causing severe eczema, eczema babies and children can be referred to an allergy specialist for further investigation including allergy testing and dietary advice.
Our Editorial Policy
Here at ScratchSleeves we aim to bring you trustworthy and accurate information. We collaborate with qualified dermatologists and doctors as well as drawing on peer-reviewed medical studies and our own experience as parents. All medical content is reviewed by a dermatologist or appropriate doctor prior to publication to ensure completeness, accuracy and appropriate use of medical language. Reviewer details can be found at the bottom of each reviewed post and also on our ‘Meet The Team’ page.
All scientific research referred to in our blog is found in peer-reviewed publications. All the eczema related medical articles we refer to are included in the GREAT database (Global Resource of Eczema Trials) managed by the Centre of Evidence Based Dermatology at the University of Nottingham. This database brings together information on all randomised control trials and systematic reviews of eczema treatments. Trials are identified using a highly sensitive, comprehensive search strategy that is compatible with standard Cochrane methodology. Cochrane is internationally recognised as the highest standard in evidence-based health care. Links to the publications we refer to are listed at the bottom of each article.
Disclaimer
The original editorial information we provide is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your doctor or other qualified healthcare practitioners regarding a medical condition. Never disregard professional medical advice or delay in seeking it in because of anything you have read on the internet.
This post has been reviewed for clinical accuracy by Dr Nikky Ellis. Nikky also has first-hand experience of navigating the NHS eczema and allergy services with her itchy son. After a number of years working in A&E, Nikky is now a GP.
Here at ScratchSleeves we don’t just share our experiences of bringing up an eczema child, we also manufacture and sell our unique stay-on scratch mitts and PJs for itchy babies, toddlers and children. We now stock sizes from 0-adult years in a range of colours. Visit our webshop for more information.
The Calm Skin Guide
Love our blog? It's also available in book format with:
- First hand accounts from parents & medical professionals
- Easy navigation
- Comprehensive index
- Additional material
Signed copies available at no extra cost
Written by:
Reviewed by:
Interesting article? Don't keep it to yourself...
Read next...
You may also find helpful...
Quick buy


Multi Buy Discount

Spend between £30 - £60 and save 5%
Spend between £60 - £120 and save 10%
Spend over £120 and save 15%
Discount automatically applied at checkout
No Quibbles Guarantee

ScratchSleeves abide by a no quibbles guarantee.
Free UK Postage

Free packing and postage on all UK orders. For overseas orders to Europe postage is from £3.50, to USA is £6.50 and to the rest of the world, from £3.75.